Buzelé, R., Barbier, L., Sauvanet, A., & Fantin, B. (2016). Medical complications following splenectomy. Journal of visceral surgery, 153(4), 277-286.
This article is a review of possible complications of a splenectomy. I chose this article because of the trauma case (SOAP #8), I recently participated in. While the patient had several other traumatic injuries, the first action taken while in the OR, besides constant resuscitation measures, was a splenectomy. I wanted to read about the complications of the procedure and what, if any, long-term measures needed to be taken for this patient due to the splenectomy. The article is from within the last five years, and directly discussed the complications that can arise from this procedure.
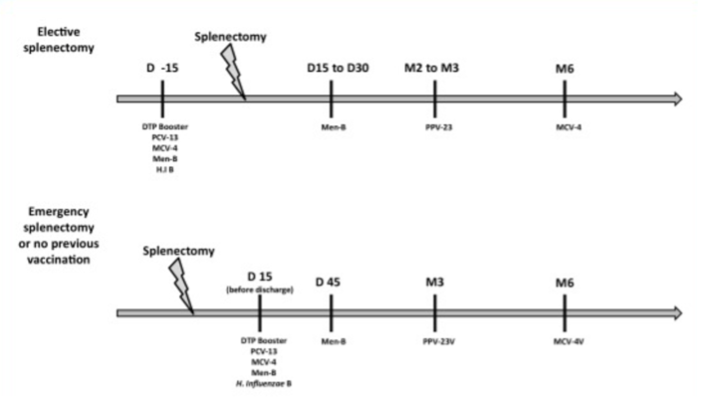
The two major complications reviewed were infections and thromboembolic events. Post-splenectomy infections are highest within two years of the surgery [50-75% from longitudinal studies], however the risk is lifelong. Encapsulated bacteria such as meningococcus, pneumococcus and haemophilus are the most concerning because the IgM memory B cells that get rid of encapsulated bacteria are primarily located in the spleen. Overwhelming post-splenectomy infection (OPSI) is another complication, which is linked to spontaneous bacteremia, and is usually due to streptococcus pneumoniae. The risk of OPSI is higher in children, those over 60, immunosuppressed, hematological malignancies or response failure to pneumococcal vaccine. Due to these infectious complications and the reduction in elimination of encapsulated bacteria, patients should receive vaccinations against these two weeks prior to surgery if planned, or at least 2 weeks after surgery in an emergent case.
Postoperative antibiotic prophylaxis can be given with IV Amoxicillin. Long-term antibiotics are still debated as vaccines are now available, but if administered, a well-tolerated and inexpensive narrow spectrum against encapsulated organisms, such as Penicillin V, is acceptable. Additionally, splenectomy patients need to be educated on the severity of a fever in their situation, as well as the complications of animal bites and need for consultation if traveling.
The thromboembolic complications post-splenectomy are due to a multitude of factors such as the hypercoagulable state of the patient, platelet activation and changes in hemodynamics. Patients are at risk for complications such as pulmonary embolism and portal vein thrombosis, however patients with multiple traumas are less likely to have in portal vein thrombosis. It is more likely in patients with cirrhosis. Interestingly, the incidence of portal vein thrombosis was higher in laparoscopy cases than laparotomy cases. There is a higher risk of deep vein thrombosis and pulmonary embolism in trauma patients with splenic injury. 67% of patients had complete resolution of thrombosis with heparin followed by 3-6 months of Warfarin. Thromboprophylaxis is still debated, but low-molecular weight heparin can be given. The takeaway of this article is that post-splenectomy patients must be followed closely to identify any complications early so immediate treatment can be implemented.


